Four years on, the Global Observatory on Health R&D continues to identify gaps and new trends in the health R&D space
[ad_1]
It is now more crucial than ever to take stock of where the world is in terms of health research and development (R&D). This is important for the worlds’ ability to address and improve all health conditions, not just for emergency preparedness.
The global COVID-19 pandemic has had an unprecedented impact on decision making in almost all aspects of life; it has emphasized the importance of adequate and appropriately-allocated funding; health R&D capacity and infrastructure; and the ability
to carry out R&D at a local level yet have the opportunity for information sharing & collaboration so as to achieve equitable population health.
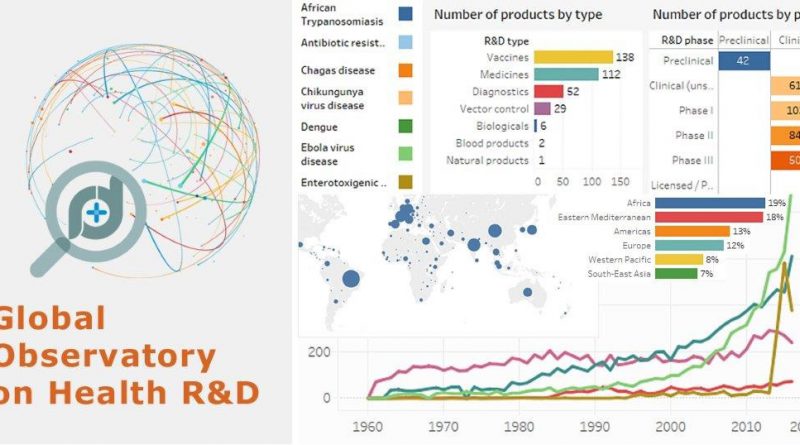
On 17 January 2017, the World Health Organization launched the Global Observatory on Health R&D (hereafter referred to as the “R&D Observatory”) to gather and analyse R&D data and information and so help governments, funders and researchers make better decisions
on investments and policy making priorities in terms of R&D and identify where the greatest needs for capacity strengthening lie. In the four years since then, the R&D Observatory has continued to identify striking gaps and inequalities in
investments – both between countries and between health issues, with frequent disconnects between disease burden and level of research activity.
Its yearly analysis and monitoring builds on a wide range of existing information and is done in close collaboration with WHO technical departments and external partners. Its output, provided in the form of interactive data visualizations that allow users to explore data further, often shows little or no improvement in addressing gaps in many
important areas.
Some key findings from the R&D Observatory’s analyses since its launch are highlighted below.
Distribution of biomedical research funding
While the total investment on grants for biomedical research for 2018 across the 10 funders that reported data to World RePORT amounted to approx.
US$ 33 billion:
- most grants were awarded for research (65%). A far smaller proportion of grants went to training (17%) and core support (8%);
- low-income countries only received 0.2% of all grants (with the majority of these low-income recipient countries being in the WHO Africa region);
- most (two-thirds) of all the grants were awarded for noncommunicable diseases (NCDs); a quarter of all investments in this area were for research relating to malignant neoplasms;
- only a tiny proportion of grants target a WHO neglected tropical disease (approx. 1%) or R&D Blueprint pathogen (approx. 0.6%).
Collaboration patterns among research institutions around the world
Analysis of biomedical research grants across the 10 funders that reported data to
World RePORT for 2018:
- 69.4% of collaborations resulted from direct grants awarded by the United States of America’s National Institutes of Health (NIH); this institution also gave the highest average grant duration;
- collaborations were most likely to be with others in the same income group. For example, grant recipients in high-income countries were most likely to collaborate with others in high-income countries;
- overall, the United Kingdom is top of the list of countries with which grant recipients collaborated.
What disease areas are being funded?
An exploration of which products are in the pipeline, what clinical trials are being conducted or what research grants are being awarded, shows that most R&D investments are going towards research on NCDs. Mirroring the funding
pattern mentioned above, only a tiny proportion of active products in the pipeline target a WHO neglected tropical disease (less than 0.5%) or a WHO R&D Blueprint pathogen (less than 0.4%).
There is some evidence of reactive research funding; for example, in 2018 around 80% of all grants for WHO R&D Blueprint pathogens were for Ebola virus disease (45%), followed by Zika virus disease (25%) and Lassa fever (9%). (Exceptionally, perhaps,
the Policy Cures Research COVID-19 tracker shows that by the end of 2020, around 9 billion US$ were pledged for COVID-19
R&D worldwide.)
How do countries compare on domestic R&D investments against global targets?
In this analysis, domestic R&D investments were measured against benchmarks (using the most recent data available by country):
- based on available evidence (from 81 countries), the data show large variations between countries. Many countries did not meet the target for their income group, while a few countries exceeded the target;
- for example, out of 29 high-income countries, only eight met or exceeded the target for high-income countries. Interestingly, Kenya (a lower middle-income country), and South Africa (an upper middle-income country) met this target – although
they are the only countries in their income groups to do so.
What is the distribution of higher education institutions offering disciplines related to research for health?
This analysis explores the relationships between country income, population, higher education institutions and opportunities for [or availability of] training in research for health:
- the number of institutions in a country is more closely related to the country’s income level than its population size or density;
- the vast majority of institutions offering a relevant discipline in 2019 were created more than 20 years ago (reflecting institutional experience). Only a small percentage of these are in the WHO Africa region (4%), the WHO Eastern Mediterranean region
(4%) or the WHO South-East Asia region (8%); - the number of institutions that offer disciplines related to research for health and provide an opportunity for research training linked to obtaining an advanced/postgraduate degree varies widely. For example, in Madagascar none of the 25 higher education
institutions provide this opportunity, while in Nigeria (also in the WHO Africa region), 76 higher education institutions (62.8%) do so.
Such information helps countries explore where they are with respect to their own targets and to other countries; it also allows countries to monitor progress towards strengthening R&D capacity. Ultimately, this will optimize delivery of health interventions
and improve access to equitable and quality health services for people across the world and so allow progress towards achieving universal health coverage and the Sustainable Development Goals.
[ad_2]
Source link